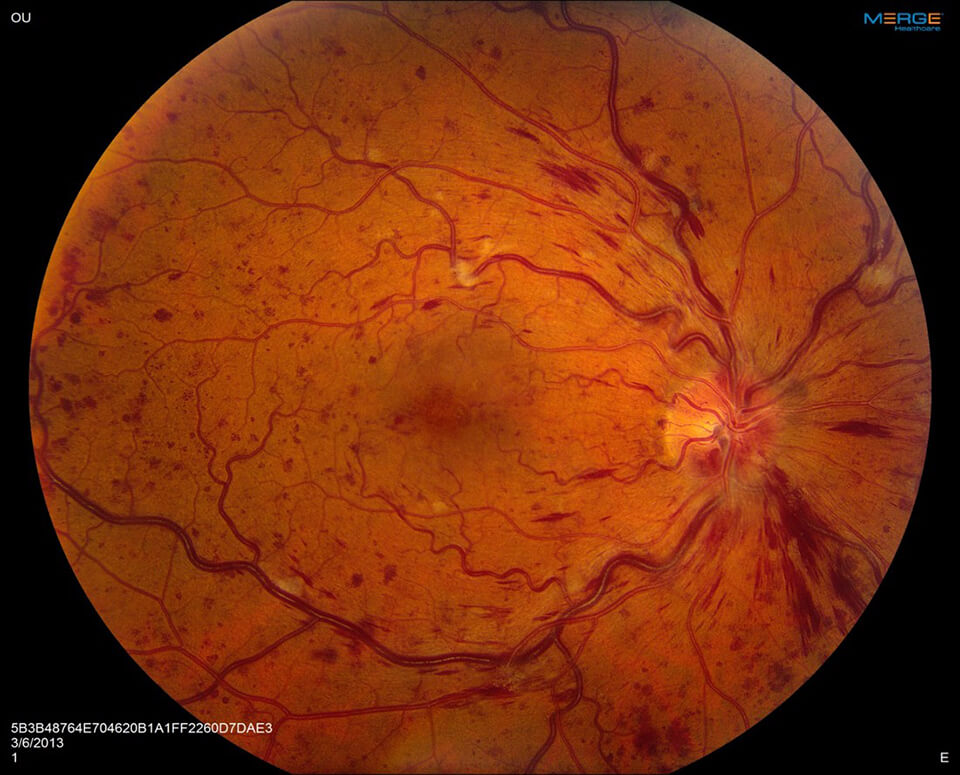
Central Retinal Vein Occlusion
What is central retinal vein occlusion (CRVO)?
The retina is the nerve tissue in the back of the eye that requires healthy blood circulation for visual function. Blood enters the retina through the central retinal artery and drains out of the retina through the central retinal vein. When the central retinal vein becomes blocked, this is called a central retinal vein occlusion or CRVO. The severity of the blockage correlates with the severity of the vision loss. There are partial and complete central retinal vein occlusions.
Symptoms of Retinal Vein Occlusion
Symptoms of a retinal vein occlusion include a sudden vision loss or blurring of vision in all or a part of the eye.
Causes of Vein Occlusion
When the vein becomes blocked, blood cannot exit, so this results in swelling and blood building up in the retina. If there is a complete blockage, the eye also becomes starved for oxygen and nutrients that come from healthy blood flow.
Is central retinal vein occlusion curable?
The prognosis for central retinal vein occlusions is, unfortunately, generally poor. The outlook is best predicted by the initial vision. Most patients who present with central retinal vein occlusions either stay the same or worsen over time. If a partial blockage is only mildly affecting vision, it can sometimes improve without treatment.
A multi-center clinical trial called the Central Retinal Vein Occlusion Study showed that patients with partial or “nonischemic” CRVO, only 10% improved, while 50% stayed the same and 1/3 worsened. In more severe cases of complete or “ischemic” CRVO, vision loss is often permanent and it is rare to get spontaneous improvement.
How Is Retinal Vein Occlusion Diagnosed?

A retinal vein occlusion is detected during a retinal exam of the eye. After a thorough medical examination of the eye, the following diagnostic tests may be conducted to confirm the diagnosis of a retinal vein occlusion:
- Pupil reflex response
- Testing of intraocular pressure
- Slit-lamp examination
- Retinal photography
- Visual field testing
- Visual acuity
- Blood tests
- Fluorescein angiogram
Treatment for Central Retinal Vein Occlusion
Although the visual prognosis is often poor for CRVO, several treatment options are available. First, it is important to identify untreated risk factors and manage those in order to decrease the risk of progression or recurrence.
Who Is At Risk For Developing CRVO?
Risk factors for central vein occlusion can include:
- A history of glaucoma
- Systemic hypertension
- Smoking
- Hyperlipidemia (high cholesterol and triglycerides)
- Diabetes mellitus
- Atherosclerosis (often characterized by prior coronary artery disease or stroke)
- Problems with blood clotting
- Blood vessel inflammation (vasculitis)
- Increased blood viscosity
This condition also has associations with oral contraceptive use. In addition, doctors often recommend aspirin therapy to try and prevent further vascular compromise. We ask that most patients with retinal vein occlusion see their internist for a thorough medical evaluation.
Complications of Central Retinal Vein Occlusion
One of the main complications of CRVO is macular edema, which is swelling in the central part of the retina. Several therapies have shown promise in managing this condition. Intravitreal administration of medications like bevacizumab (Avastin) that block Vascular Endothelial Growth Factor (VEGF) may have a role. Other treatments for macular edema from CRVO include intravitreal steroid administration. A sustained-release steroid implant is available as well.
In the event that CRVO becomes severe, abnormal blood vessels may develop in the eye. Also, these blood vessels can grow into the drainage system of the eye, causing a severe form of glaucoma. Consequently, this can lead to pain and loss of all visual function. If your central retinal vein occlusion is in the more severe category, your eye will need to be monitored more closely and frequently for this, especially in the first 6 months after development. We may combine laser treatment with anti-VEGF if we detect abnormal blood vessels. Vitrectomy surgery is sometimes necessary. Glaucoma surgery may also be necessary if the problem becomes worse.
Schedule a Consultation
To learn more about diabetic retinopathy, please call (855) 515-2020 to schedule a consultation.
We are proud to serve the communities of Minneapolis/St Paul, Brainerd, Duluth, Glencoe, Mankato, St. Cloud, and more.

